At the Veterans Affairs (VA) Ann Arbor Healthcare System, patient care is shaped by a deliberate, team-based approach that brings together clinicians, staff, and specialists across disciplines. This model is rooted in the VA’s national shift toward Patient-Aligned Care Teams, or PACT, a framework introduced to strengthen primary care by centering it around whole-person, lifelong health and wellness. Developed to move beyond episodic treatment, PACT emphasizes prevention, access, and coordination, ensuring that care is organized around veterans rather than individual appointments or services.
Within this structure, each veteran partners with a dedicated care team that works collaboratively to address medical needs, personal goals, and overall well-being. These care teams are made up of physicians, RNs, LPNs, MAs, PharmDs, social workers, advanced medical support assistants (AMSAs), and more. The PACT model provides the framework for coordinated, consistent care, but it is the people within that system who bring it to life through trusted relationships, clear roles, and a shared commitment to team-based care.
Dr. Rajesh Mangrulkar, MD, a primary care physician at the VA and director of the Michigan Center for Interprofessional Practice and Education (CIPE), sees this approach as foundational to high-quality care, and it's why he was drawn to the work of CIPE. The Center works across the University of Michigan’s three campuses and Michigan Medicine to strengthen interprofessional education and collaborative practice. By aligning the training of health professionals with real-world care delivery, the center supports a workforce prepared to meet the complex needs of patients.
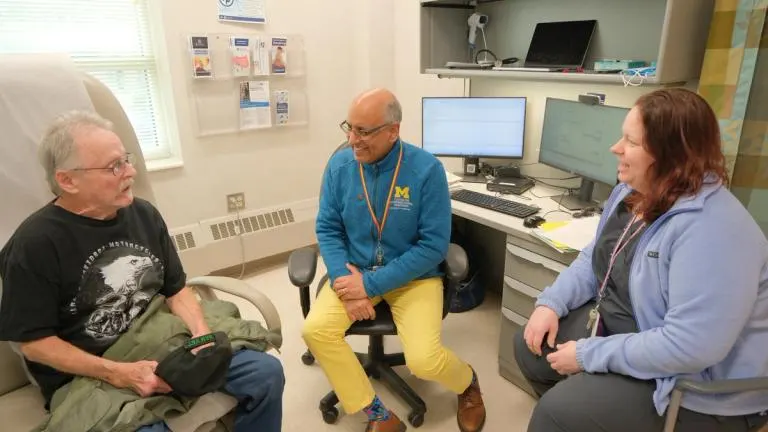
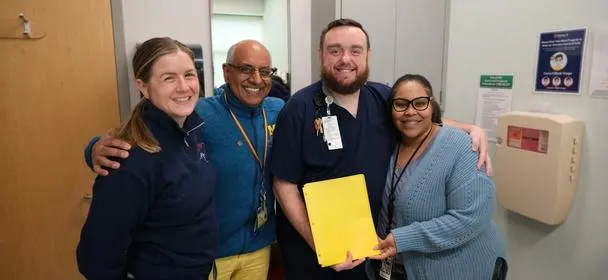
Photo: (L-R) Mr. Timothy Jones speaks with Rajesh Mangrulkar, MD, and Keri Pranga, RN care manager, during a check-up.
Credit: John McGraw, Michigan Center for Interprofessional Practice and Education (CIPE)
That commitment is reinforced through Dr. Mangrulkar’s daily work with his own primary care team at the VA, where coordinated, team-based care is essential to managing complex patient needs. In fact, he views his days at the VA as the most meaningful work he gets to be part of. "I didn't go to medical school to be a director or dean," Dr. Mangrulkar says, "but being part of this amazing team is what I yearned for throughout my education and training."
Taken together, these experiences have shaped how Dr. Mangrulkar thinks about what effective, patient-centered care should look like at its best. Dr. Mangrulkar views the PACT model as the ideal approach to healthcare for all patients, not only those served through the VA system. “When teams are connected and communicating well, care becomes more responsive and more effective,” Dr. Mangrulkar said. “That collaboration shows up in every patient interaction.”
Patients feel that impact directly. Mr. Timothy Jones, who has received care at the VA for several years, describes his experience as consistently positive. “The care has been great,” he said. “Everyone is attentive, and the team really works together.” Mr. Jones credits much of that experience to the people he interacts with most often, including his nurse, Adam, front desk staff member Tiffany, and pharmacist, Holly Thompson. “They make everything run smoothly,” he said. “You feel supported the whole time you’re here.”
Photo: (L-R) Tiffany Parker, AMSA, hands a patient document to Rajesh Mangrulkar, MD, as he conducts a check-up with Mr. Albert Keskeny.
Credit: John McGraw, Michigan Center for Interprofessional Practice and Education (CIPE)
Another patient, Mr. Albert Keskeny, shared a similar perspective. “This is the best facility I’ve been to,” he said. “From the moment I walked in, people were welcoming and helpful.” He described how staff members take time to guide patients through the space and answer questions. “If you’re unsure where to go, someone walks you there. That makes a difference. You feel like people actually care.”
For many, the patient experience begins at the front desk. Tiffany Parker, advanced medical support assistant (AMSA), plays a key role in coordinating care and supporting both patients and clinicians throughout the day. Her responsibilities range from scheduling and documentation to communication and problem-solving, but her role also relies heavily on attentiveness and judgment.
“You get to know your patients,” Parker said. “You notice when something is off.” She recalled a moment when she observed a patient experiencing abnormal breathing. Recognizing the urgency, she alerted the clinical team immediately. The patient ultimately required emergency care. “That’s why being present and paying attention matters,” she said. “We’re all watching out for our patients.”
Photo: Tiffany Parker, AMSA, speaks to the teamwork displayed at the Ann Arbor VA Healthcare System.
Credit: John McGraw, Michigan Center for Interprofessional Practice and Education (CIPE)
That sense of shared responsibility extends across the care team. Parker emphasized that strong working relationships make it easier to respond quickly and effectively. “We talk through things, we help each other, and we trust one another. That teamwork is what keeps everything moving.”
Nikki Culkowski, licensed practical nurse (LPN), echoed that sentiment. She described the VA as a setting where collaboration is built into daily practice. “There’s a level of teamwork here that you don’t always see,” she said. “You can walk down the hall and connect with a pharmacist, a social worker, or a mental health provider without barriers.”
As an LPN, Culkowski plays a central role in patient education, care coordination, and clinical support. She works closely with physicians and other team members to ensure that patient concerns are addressed efficiently and thoughtfully. “We get to know our patients well,” she said. “That helps us anticipate their needs and communicate clearly as a team.”

Photo: (L-R) Nikki Culkowski, LPN, and Shannon Quesada, RN, review their team's schedule.
Credit: John McGraw, Michigan Center for Interprofessional Practice and Education (CIPE)
Each morning begins with a brief team huddle that helps align care for the day ahead. These huddles take place at the start of each shift change and bring together LPNs, RNs, physicians, administrative staff, and other clinical staff. When he is on site, primary care physician Dr. Mangrulkar participates in the discussion, focusing on scheduled appointments, anticipated patient needs, and role clarity so everyone on the team is prepared to deliver coordinated care. As Culkowski explains, “We are a detail-oriented team. We look at the needs of our patients, but also at one another’s needs.”
These regular huddles are a key way the PACT model comes to life. By meeting consistently and communicating openly, team members build trust through shared accountability and mutual respect. Questions are surfaced early, insights from different disciplines shape care plans, and collaboration continues beyond the huddle through follow-ups, referrals, and ongoing communication across the team. Team communication channels include face-to-face, by phone, TEAMS messaging, or alert messages through the electronic health record. This steady rhythm of teamwork strengthens relationships within the care team and helps ensure veterans receive personalized, connected care centered on their goals.
Shannon Quesada, RN, described the environment as one where collaboration is expected and supported. “We work together constantly,” she said. “If something comes up, someone always knows what to do or who to call. We rely on each other, and that trust makes a difference for patients.”
Across roles and disciplines, there is a shared sense of purpose rooted in service to veterans. Many staff members describe their work as a way to give back and to honor those who have served. For patients like Mr. Jones and Mr. Keskeny, the result is care that feels organized, attentive, and personal. For the clinicians and staff, it is a workplace shaped by collaboration and mutual respect. “It is a very special, unique place because of the camaraderie that we’ve fostered across our disciplines,” said Culkowski.
Together, the team demonstrates how intentional interprofessional teamwork can strengthen care delivery and create a more supportive experience for everyone involved. Dr. Mangrulkar yearns to broaden the practice of team-based care and its outcomes to patients everywhere–not just those in the VA.